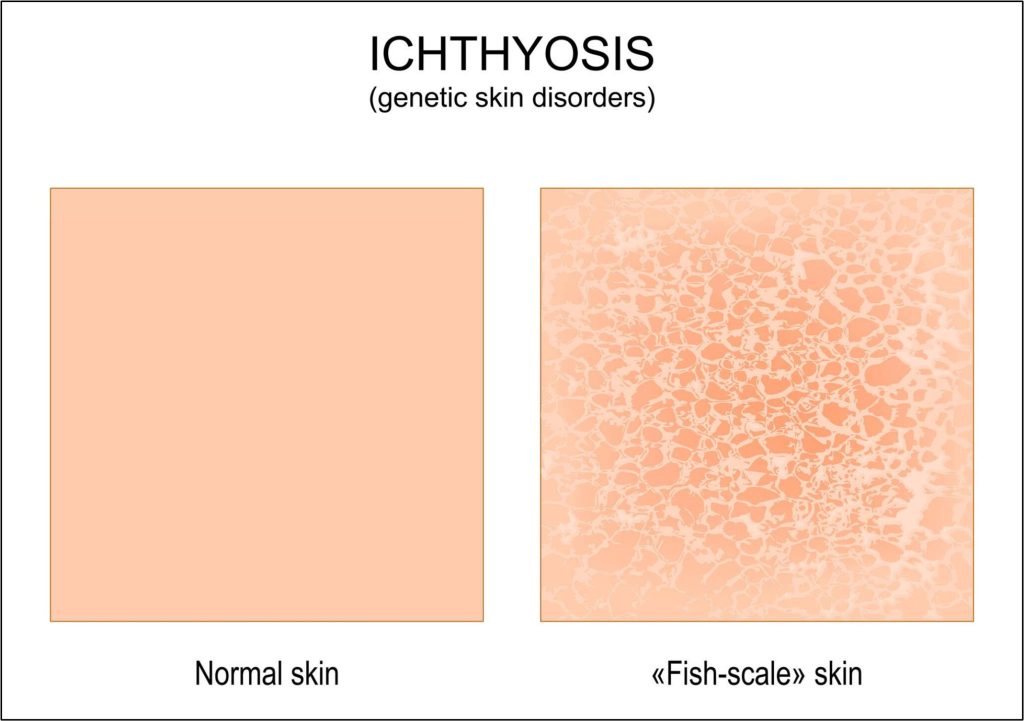
Skin is the defensive shield and image of our existence that expresses the secrets of our genes. Ichthyosis is a unique challenge that illustrates the stories of rare beauties. Skin is a protective barrier, yet it is a delicate organ that can easily crack due to external or internal events, microorganisms, or genetic disorders. Ichthyosis is a rare and unknown illness that causes scaling of the skin and shows a resemblance to fish. Several indicators of ichthyosis are apparent, but it comes with similar discomfort and irritation.
If you ever experience this disease, let me explain its genetic causes and treatment of ichthyosis.
What is Ichthyosis?
Ichthyosis, known as fish scale disease, is an inherited condition exhibiting dry, thick, and scaly skin. As ichthyosis is a genetic disorder, it can only be inherited from parents to offspring; however, numerous other factors may also be responsible for this condition occurring. For instance, acquired ichthyosis is a type of ichthyosis that develops after taking certain medications or due to other medical conditions. Acquired ichthyosis is a non-heritable form of ichthyosis.
Forms of Ichthyosis
There are more than 20 forms of ichthyosis, which can affect several areas of the human body, including arms, torso, face, legs, buttocks, ears, or the whole body. Ichthyosis commonly affects the skin, but other forms can also impact internal organs. There are several defined manifestations of ichthyosis, but ichthyosis vulgaris is the most common form among others, contributing to almost 95% of ichthyosis cases. General symptoms associated with almost all forms of ichthyosis include dry, thick, and scaly skin.
Types of Ichthyosis
There are five major types of ichthyosis, including
Ichthyosis vulgaris
It’s the most common disease and appears in the first year after birth, indicating dry and flaky skin.
lamellar ichthyosis
It’s a by-birth disease. When an infant is born, his entire body is covered with a clear membrane known as a collodion membrane. After some weeks, this membrane peels up and dark plate-like scales show off over the entire body.
Epidermolytic hyperkeratosis
When an infant is born, fragile and blistered skin covers the whole body. As time passes, these blisters disappear, and scaling develops on the skin.
X-linked Ichthyosis
This disease usually belongs to males and develops at the age of 3 to 6 months; the scaling appears on the neck, legs, trunk and lower face.
Harlequin ichthyosis
This disorder is also seen at birth age, and it affects the facial shape of a child, and the movement of joints is also limited.
Why does ichthyosis vulgaris happen?
Ichthyosis vulgaris, also known as ichthyosis simplex, is the most commonly occurring form of ichthyosis. That’s why it is also referred to as common ichthyosis.

Our skin cells typically divide, and after completing their life span or due to any injury, they die and shed off from the skin’s surface. The life span of the human skin cells is two to four weeks. After this, skin cells die and are replaced by new skin cells or layers. During this process, old or dead skin cells must be removed from the skin surface to accommodate new ones. However, in the case of ichthyosis vulgaris, rather than falling off the skin surface, the dead skin cells start accumulating on the skin’s surface, causing the formation of scales, giving a scaly and thick skin appearance. In short, the new cells are being produced regularly, and dead cells are not shedding, which is what basically happens in ichthyosis vulgaris.
Facts about ichthyosis vulgaris
- “Prickly itch” is among one of the most common conditions associated with ichthyosis vulgaris.
- Sweat prevents overheating of the body. However, thick scales in patients with ichthyosis vulgaris might block skin pores, thus minimizing the sweating that leads to excessive itching due to overheating.
- Ichthyosis vulgaris is not a life-threatening condition, and symptoms usually fade away with age. Sometimes, this skin disorder may lead to worse illnesses like testicular cancer and abnormal sperm count in males.
- Individuals taking certain medications like cimetidine, clofazimine, and nicotinic acid are also reported to develop acquired ichthyosis vulgaris.
- Other medical conditions like sarcoidosis, leprosy, some cancers, underactive thyroid gland, and kidney failures also tend to cause acquired ichthyosis vulgaris in those patients.
- Almost 50% of individuals with ichthyosis vulgaris also develop other skin conditions like eczema, asthma, and other allergies.
Why is ichthyosis known as an inherited disorder?
Each human cell contains DNA as its genetic material, which holds information hubs in the form of genes. For instance, there are specific genes for eyes, skin, hair colors, or height and the tendency to develop certain diseases; all data are stored on genes. Genes then pass down from parents to offspring, carrying vital information for the normal functioning of the human body, giving distinct physical and biological traits. Each gene codes for a specific protein responsible for sustaining a particular function. Somehow, genes are prone to mutations, which means that the structure or sequence of the genes can be changed through internal or external factors. Mutated genes become defective and unable to code appropriately; instead, they code an entirely different protein, which is faulty and causes potential disturbances in the human body, resulting in a disease or disorder. If these mutated genes are transferred from parents to offspring, they result in a genetic disorder.
Ichthyosis vulgaris is an autosomal inherited disorder. Ichthyosis vulgaris occurs due to mutations or changes in a specific gene. FLG gene is responsible for synthesizing a protein filaggrin, mutates and becomes defective. Filaggrin serves as a barrier for skin against allergens, stabilizes skin pH, and assists in shedding dead skin cells. It also plays a crucial role in retaining water or moisture content in the skin. Individuals with ichthyosis vulgaris have minimal to no filaggrin in their skin, resulting in dryness and thick scales on the skin.
Symptoms of Ichthyosis Vulgaris
Dry, rough, thick, and scaly skin, a condition termed xerosis, which gives an untidy look
- The scales may be white, grey, or dark brown. Edges of scales on the skin become curly, giving an ugly appearance, especially on the face and hands.
- Less perspiration causes overheating of the body.
- Skin tight makes movement hard
- Problems while bending the joints and listening
- Associated conditions like atopic dermatitis or eczema are frequent in people who are suffering from ichthyosis vulgaris
- The risk of asthma, food allergies, and rhinitis is also increased
- Hyper-linearity that is, defined lines on palms and soles
- Keratosis pilaris is the appearance of itchy, red, and inflamed small bumps, most probably on the face, thighs, waist and buttocks
The symptoms of dry, scaly skin are absent at the time of birth; however, they start appearing from childhood, usually from the age of three months to five years. Additionally, symptoms of ichthyosis can develop at the adult stage or even later in life.
Diagnosis of Ichthyosis Vulgaris
Ichthyosis vulgaris is diagnosed by observing the patient’s physical appearance and condition and asking for personal and family history. Besides that, skin biopsy, a test in which a small portion of the skin is examined under a microscope, and skin tissue testing are effective diagnostic methods.
Treatment of Ichthyosis Vulgaris
Unfortunately, this condition has no cure, as it is inherited. However, other remedies help alleviate the intense symptoms.
- Moisturizing the skin using certain emollients and topical retinoids like tretinoin can alleviate skin dryness. Using moisturizers can retain the water content in the skin.
- Take a bath at least two times a day.
- The oral or skin medications that a doctor recommends to you
- Apart from emollients, alpha-hydroxy acids like lactic acid, glycolic, and pyruvic acid are also recommended for keeping skin moist and hydrated.
- If there is a massive buildup of scales, they can be removed by keratolytic-like salicylic acids. Salicylic acid causes skin cells to break down in the uppermost skin layer, creating clear skin.
Final Thoughts
Ichthyosis affects about 1 in 1000 people globally. It was first discovered in 1900 by Sir William Osler. Genetic mutations are the major cause of this disease, and it appears as dry, scaly skin or thickened skin in infants. It’s not a chronic disease but could lead to some complications such as dehydration, skin allergies or even asthma.
Frequently Asked Questions – FAQs
Does ichthyosis ever go away?
Mostly, ichthyosis is not cured, but some treatments may include the use of emollients, ointments or bath oils.
Does ichthyosis hurt?
When it reaches severe cases, it leads to deep, painful cracks on hands and feet that hurt the patients.
Who is at risk of ichthyosis?
This disease usually passes from parents to offspring. But sometimes, rare people are those who are the first person in their family to get this disease.
About the Author
Dr Madilyn Adams is a PhD in molecular medicine from Harvard University and has been working as a medical blogger for seven years.